 OUR LOCATIONS
Call to book 201.523.9590
OUR LOCATIONS
Call to book 201.523.9590
 OUR LOCATIONS
Call to book 201.523.9590
OUR LOCATIONS
Call to book 201.523.9590

We put a lot of strain on our spinal column, and over time, the soft discs within them can become injured, whether it’s because of accidents, overexertion, or simply getting older. This can lead to a variety of issues, but among the most prevalent are bulging and herniated discs, which are the main causes of lower back pain. In turn, these conditions can cause nerve damage to the affected areas of the spinal canal, eventually affecting the entire body.
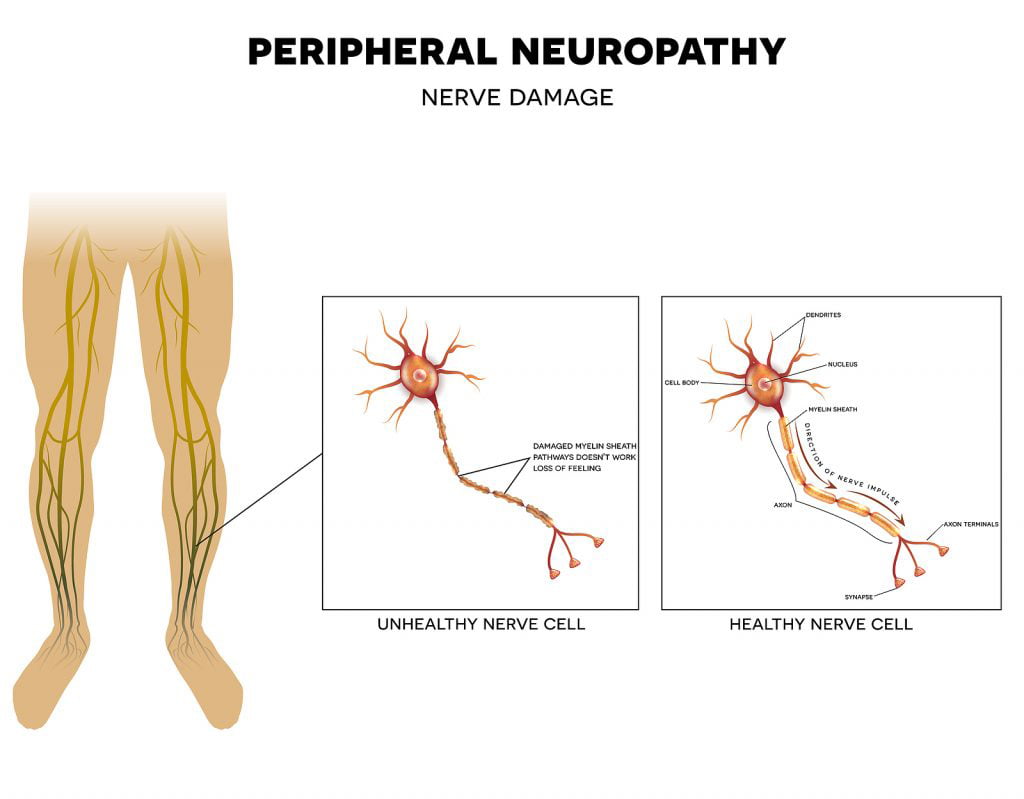
So can bulging discs cause peripheral neuropathy? There are a number of different conditions that can result in peripheral neuropathy, but back neuropathy usually occurs as a result of nerve compression. Neuropathy can be brought on by a variety of different injuries. Bulging and herniated discs are among the most prevalent causes of neuropathy in the back. The pinched nerve is compressed by the disc, which causes it to transmit pain signals to the brain.
Proximal peripheral neuropathy occurs when a nerve root in the spinal column is damaged, irritated, diseased, compressed, or otherwise affected. One of the most prevalent peripheral neuropathies in the body is a radiculopathy, which is caused by bulging discs.
This proximal peripheral neuropathy contributes to several occurrences of leg pain, numbness, tingling, loss of muscular function in the foot or leg, or loss of coordination. The damaged nerve root at the back may get irritated or compressed, which would cause all of these symptoms.
Even though peripheral nerve pain usually subsides on its own, it can become chronic in some cases. Peripheral nerve disorder is typically the result of an accident or trauma that impacts or compresses a nerve, permanently destroying it.
For instance, a herniated or bulging disc may press against a nerve root in the spinal cord, causing the brain to receive signals of neuropathic pain. The pinched nerve may no longer be compressed by the bulging or herniated disc over time, but the spinal nerve tissue may still sustain damage and continue to malfunction and transmit a pain signal to the brain.
Compared to other types of pain, neuropathy pain is distinctive. For instance, when a bone is broken, the nerves near the fracture send a pain signal to the brain. However, the damage in neuropathic pain is limited to the nerves themselves.
Most often, nerve compression and dysfunction that results from trauma or injury is what leads to neuropathy. When the initial trauma or injury has truly healed, the compressed nerve becomes hypersensitive and starts to trick the brain into believing that there is still pain. The central or peripheral nervous systems are where most injuries first manifest.
It’s important to note that the symptoms of neuropathy vary according to what type of nerve is affected and where the damaged nerve is located. Acute neuropathy is characterized by the quick onset of symptoms, whereas chronic neuropathy is characterized by a slow, progressive onset.
The signs and symptoms of neuropathic pain can be unpredictable and differ greatly from person to person. A particular stimulus can cause pain, or it can happen on its own. When a sudden impact occurs, not just the immediate area but also the area around the trauma site may be affected.
While some people endure pain continuously, others might just occasionally feel it. Movement is frequently painful for a person with neuropathic pain, which limits their mobility. The symptom of muscle deterioration brought on by inactivity might further limit physical functioning. Many neuropathies prevent their sufferers from working.
The following are several ways to describe back pain or other pain associated with neuropathy:
Skin in the painful area may experience some discoloration, which can appear more pink or red than usual. In some occurrences, the skin may seem blue or spotted. Usually, variations in blood flow cause changes in color. Additionally, the symptom of inflammation could occur in some people.
Sleep disturbances and depression are common in neuropathic pain sufferers, and both of these conditions can make pain feel worse. To treat all facets of the person’s health, a multifaceted approach to pain management may be effective.
It may be possible to use sensory tests to determine how the patient reacts to various forms of physical contact. The following are some uncommon experiences that people with neuropathic pain may encounter:
Neuropathy is a disorder that can result from any condition or trauma that compresses a nerve. Injuries to the compressed nerve root in the spinal cord that might cause neuropathy include bulging or herniated discs. In addition to these, there are additional types of neuropathic pain that start in the back or on a spinal nerve.
Injections, diabetes, complex regional pain syndrome, injuries, diseases, substance addiction, or exposure to toxins are some other conditions that can result in neuropathy. However, neuropathy’s root cause isn’t always obvious.
Some peripheral neuropathies progress slowly, over months or even years, whereas others advance quickly and only become worse. Neuropathies come in more than a hundred different varieties, and they can all manifest in various ways. Depending on the nerve or nerves that are damaged, and their underlying cause, the way your condition progresses and when symptoms begin can vary greatly.
Early intervention is crucial because if symptoms aren’t treated quickly, more aggressive treatment may be required. Central sensitization is a condition that develops when a person experiences severe pain over an extended period of time and results in alterations to the central nervous system that cause the body to be more sensitive to even the slightest touch.
Delays in treatment may increase the likelihood of various health complications, much like with other types of chronic pain. Untreated neuropathy is linked to a number of health conditions, including depression, anxiety, sleep problems, and the inability to work or engage in other activities. When a nerve root in the spinal column is injured, irritated, diseased, pinched, or otherwise impacted, proximal peripheral neuropathy develops.
Blood tests, and diagnostic procedures including magnetic resonance imaging (MRI), nerve conduction examinations, and electromyography, along with other methods, can be utilized to identify the cause or rule out potential causes. The results of tests can be useful in determining the best course of treatment for pain relief.
Neuropathy can occasionally be effectively treated and even cured in some situations. However, not all neuropathies are curable. Treatment in these situations aims to manage pain relief and control the symptoms as well as stop additional nerve damage. The following are some treatment options for peripheral neuropathy:
A medical professional may prescribe the necessary medication for a patient who is experiencing pain from a nerve disorder. Different medications are frequently used to treat neuropathic pain because, unlike other types of pain, it rarely gets better when treated with over-the-counter analgesics like paracetamol and ibuprofen.
Usually, you should start them at the lowest dose and gradually increase it until you start to feel the effects. While higher doses may be more effective at controlling pain, they also carry a higher risk of negative side effects.
Pain can be managed with the use of medication. Many different medications incorporate chemicals that regulate the pain signaling pathways in the central and peripheral nervous systems to assist reduce pain. A pain specialist may prescribe you the following medications:
During this procedure, electrodes are applied to the skin at or close to the pain-causing nerves. Your skin receives a soft, low-level electrical current from the electrodes. Your therapist determines your treatment plan, including the frequency and duration of the procedure. In order to prevent pain signals from reaching the brain, TENS treatment works by interrupting pain signals.
Patients might be inclined to attempt alternative remedies because peripheral neuropathy can be a very uncomfortable and bothersome nerve disorder that conventional treatments may only partially alleviate.
Alternative treatments for neuropathic pain include massage therapy, acupuncture, alpha-lipoic acid, physical therapy, meditation and yoga, chiropractic care, and psychotherapy. Consult your doctor to see if any of the following treatments could help you address the underlying cause of your neuropathy.
The diagnosis and management of neuropathic pain can both be challenging. To acquire a proper diagnosis of your pain condition, consult a certified back specialist. A medical professional can perform specialized tests, eliminate serious underlying problems like bulging or herniated disks and create a successful treatment strategy for your neuropathic pain.
At The Spine And Rehab Group, our specialists have extensive training in the diagnosis and management of back pain. As a leading medical facility in New York City, we take pride in our dedication to providing excellent patient care and assisting patients in overcoming any medical conditions they may experience. Get in touch with one of our clinics today to learn more about our services.



